When a patient can’t communicate with their healthcare provider due to a language barrier, critical details get lost. Symptoms go unreported. Treatment instructions become unclear. Medical errors happen. Patient interpretation bridges this gap by enabling clear, accurate communication between providers and patients who speak different languages or use sign language. For healthcare facilities, understanding how these services work isn’t optional, it’s essential for delivering safe, compliant care.
This article breaks down what patient interpretation actually involves, the different types of language assistance available (video, phone, and in-person), and why these services matter for both clinical outcomes and legal compliance. You’ll also learn best practices for implementing interpretation in your facility and how to choose the right service model for your needs.
At Languages Unlimited, we’ve provided medical interpretation services since 1994, supporting healthcare providers across all 50 states with over ten thousand qualified interpreters covering hundreds of languages and dialects. Whether you need Video Remote Interpreting for a quick patient consultation or on-site ASL interpretation for a complex procedure, we understand what’s at stake when communication breaks down in clinical settings.
What patient interpretation means in healthcare
Patient interpretation refers to the real-time conversion of spoken or signed language between healthcare providers and patients during medical encounters. An interpreter facilitates communication by listening to what one party says, then rendering that message in the other party’s language while maintaining accuracy and neutrality. You see this service in action when a Spanish-speaking patient discusses symptoms with an English-speaking doctor, or when a deaf patient uses an ASL interpreter to understand discharge instructions. The interpreter handles verbal exchanges, questions, and responses as they happen, making the conversation possible.
The basic function of medical interpreters
Medical interpreters do more than swap words between languages. They convey medical terminology, cultural context, and emotional nuance while remaining invisible to the conversation itself. When your patient says they have "coraje" in Spanish, a qualified interpreter knows this can mean anger or a folk illness concept, and they’ll clarify which meaning applies. The interpreter maintains first-person communication, so when your patient speaks, the interpreter says "I have pain" rather than "She says she has pain." This direct approach keeps the therapeutic relationship between you and your patient intact.
Professional medical interpreters follow strict protocols. They interpret everything said by both parties without adding, omitting, or summarizing information. They maintain patient confidentiality under HIPAA regulations and disclose any potential conflicts of interest before the session begins. If they don’t understand a term or need clarification, they’ll speak in third person to request it, then return to first-person interpretation once the issue resolves.
Who requires interpretation services
You’ll encounter patients who need interpretation services across multiple populations. Limited English Proficient (LEP) patients make up the largest group, speaking primary languages ranging from Spanish and Mandarin to Karen and Hmong. According to the U.S. Census Bureau, over 25 million people in the United States speak English less than "very well," and many of these individuals seek medical care where English dominates. Your facility must provide meaningful access to these patients under federal civil rights laws.
Deaf and hard-of-hearing patients represent another critical population requiring interpretation. These patients use American Sign Language (ASL) or other signed languages as their primary mode of communication. You can’t assume a deaf patient can lipread or communicate effectively through written notes. ASL has its own grammar and structure, distinct from English, which means a qualified sign language interpreter becomes necessary for complex medical discussions, informed consent, and treatment planning.
Providing interpretation services isn’t just about being helpful; it’s a legal requirement under Title VI of the Civil Rights Act for any facility receiving federal funding.
How interpretation differs from translation
You’ll sometimes hear people use "interpretation" and "translation" interchangeably, but they describe different services. Interpretation handles spoken or signed language in real time during conversations, appointments, or procedures. Translation works with written documents like consent forms, discharge instructions, or medical records. An interpreter must process and convey meaning instantly while managing the flow of dialogue. A translator has time to research terminology, consult references, and refine the final text for accuracy.
The skill sets differ significantly between these roles. Interpreters need quick cognitive processing, strong short-term memory, and the ability to manage fast-paced exchanges while maintaining composure under pressure. Translators require deep knowledge of medical terminology in both languages, attention to detail in written formats, and familiarity with formatting conventions for medical documents. Your facility needs both services, but you’ll deploy them in different situations based on whether the communication happens verbally in the moment or through written materials that patients take home.
Why patient interpretation matters
Patient interpretation directly affects three critical areas in your healthcare facility: clinical safety, legal compliance, and patient trust. When you provide qualified interpretation services, you reduce medical errors, meet federal requirements, and improve health outcomes for your diverse patient population. Without these services, you risk misdiagnosis, treatment complications, and potential liability while alienating the communities you serve.
Clinical safety and medical accuracy
Miscommunication in healthcare settings leads to preventable medical errors that can harm or kill patients. When you rely on untrained staff members or family members to interpret, critical symptoms get lost or distorted. A patient’s chest pain becomes "stomach discomfort." A medication allergy goes unreported. Your clinical decisions depend on accurate information, and professional interpreters ensure nothing gets missed or misunderstood during the patient history, physical examination, or treatment discussion.
Research shows that patients who receive care with professional interpretation services have comparable health outcomes to English-proficient patients, while those without interpretation face significantly worse results. You see this impact across the care continuum, from initial diagnosis through medication adherence and follow-up appointments. When your diabetic patient understands how to check blood sugar levels and adjust insulin doses, they avoid emergency room visits and long-term complications that professional interpretation helps prevent.
Federal compliance obligations
Your facility must provide meaningful access to patients with limited English proficiency under Title VI of the Civil Rights Act if you receive federal funding. This includes Medicare, Medicaid, or other federal financial assistance. The obligation extends beyond just offering interpretation services; you need to inform patients about available language assistance, provide qualified interpreters at no cost, and ensure timely access to these services throughout every stage of care.
Facilities that fail to provide adequate interpretation services face investigations, compliance reviews, and potential loss of federal funding.
The Department of Health and Human Services Office for Civil Rights enforces these requirements and investigates discrimination complaints. You can’t ask patients to bring their own interpreters or charge them for language services. Your facility bears the responsibility and cost of removing language barriers that prevent equal access to healthcare.
Patient engagement and satisfaction
Patients who communicate through professional interpreters report higher satisfaction scores and greater trust in their healthcare providers. They ask more questions, express concerns openly, and participate actively in treatment decisions when language barriers disappear. This engagement translates into better adherence to treatment plans, fewer missed appointments, and improved long-term health outcomes for your patient population.
Building therapeutic relationships requires clear communication. When you work with interpreters who maintain confidentiality and neutrality, your patients feel respected and understood. They return to your facility for ongoing care and recommend your services to family members who face similar language barriers.
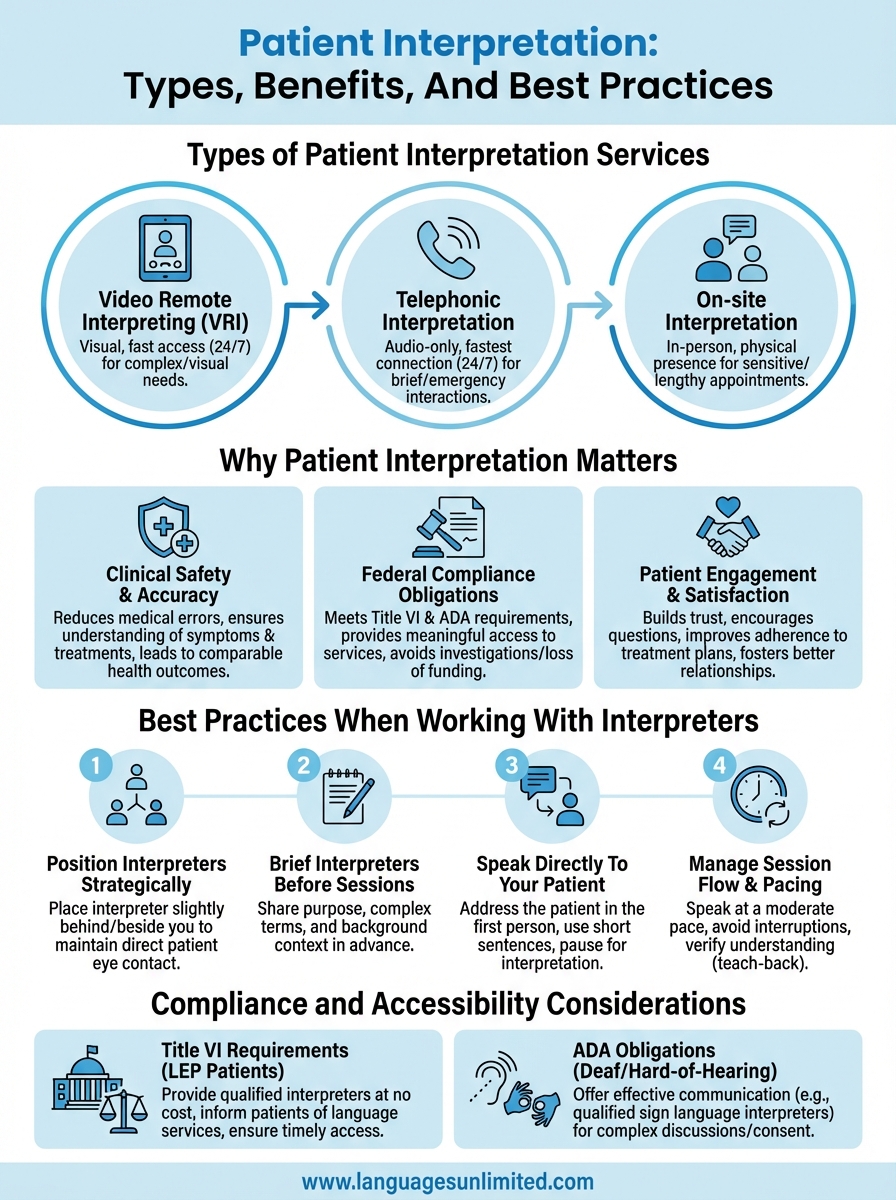
Types of patient interpretation services
You have three primary modes of patient interpretation to choose from when supporting patients with language barriers: video remote interpreting, telephonic interpretation, and on-site interpretation. Each mode serves different clinical scenarios based on factors like urgency, complexity, visual requirements, and available resources at your facility. Understanding how these services work helps you deploy the right interpretation method for each patient encounter, whether you need immediate access for an emergency department visit or scheduled support for a prenatal consultation.
Video Remote Interpreting (VRI)
Video Remote Interpreting connects you with professional interpreters through live video conferencing technology using tablets, computers, or dedicated devices. You initiate the call when your patient arrives, and an interpreter appears on screen within seconds to facilitate the conversation. The interpreter sees both you and your patient, allowing them to observe body language, facial expressions, and any visual materials you display, such as diagrams or medication bottles. This visual component makes VRI particularly effective for complex medical discussions where nonverbal cues matter.
VRI works well in hospital settings, clinics, and urgent care facilities where you need quick access to interpreters across multiple languages. You can connect with Spanish, Mandarin, Arabic, or Vietnamese interpreters without maintaining on-site staff for each language. The technology allows you to switch between languages instantly if your patient’s family member needs interpretation in a different language during the same visit.
Telephonic interpretation
Telephonic interpretation provides audio-only interpretation through phone calls that connect you with professional interpreters in seconds. You dial a service number, select your needed language, and an interpreter joins the call to facilitate conversation between you and your patient. This mode offers the fastest connection times and works from any location with phone access, making it ideal for emergency situations or when you need immediate language support without visual requirements.
Telephonic interpretation gives you 24/7 access to interpreters in hundreds of languages, including rare dialects that may not have local interpreters available.
You’ll find telephonic interpretation useful for brief interactions like medication instructions, appointment scheduling, or initial triage assessments. The service costs less than on-site interpretation while maintaining professional quality standards, though it lacks the visual context that some clinical situations require.
On-site interpretation
On-site interpretation brings qualified interpreters physically present in your facility during patient appointments, procedures, or consultations. These interpreters work in consecutive or simultaneous modes depending on your needs. In consecutive interpretation, the interpreter waits for natural pauses to convey messages between languages. In simultaneous interpretation, the interpreter speaks almost concurrently with the speaker, typically used for longer sessions like therapy appointments or complex procedures where continuous flow matters.
You schedule on-site interpreters in advance for planned appointments, surgeries, or discharge planning sessions that require extended interpretation support. This mode suits situations where personal presence enhances trust, such as mental health counseling, end-of-life discussions, or pediatric care where family dynamics play a significant role. On-site sign language interpreters also serve deaf patients who require ASL interpretation for medical procedures or consultations.
How to choose the right interpreting mode
You need to match your interpretation mode to the specific clinical situation, considering factors like urgency, complexity, and available resources at your facility. The right choice depends on whether your patient needs immediate emergency care or scheduled prenatal counseling, whether visual communication matters for the medical discussion, and what interpretation services your facility can access. Making this decision systematically ensures you provide effective language support while managing costs and maintaining quality standards across your patient population.
Clinical complexity and visual needs
Your clinical scenario determines whether visual communication plays a critical role in patient interpretation. You should choose VRI or on-site interpretation when the encounter involves demonstrating procedures, showing anatomical diagrams, reviewing medication labels, or discussing wound care where pointing and visual reference matter. Physical therapy sessions, surgical consent discussions, and diabetes education require interpreters who can see what you’re showing the patient and help coordinate physical demonstrations.
Telephonic interpretation works effectively for straightforward verbal exchanges like medication dosing instructions, appointment confirmations, or brief triage assessments where visual context adds limited value. You can use phone interpretation when checking on a patient’s post-discharge progress or scheduling follow-up appointments. Mental health counseling typically requires on-site or video interpretation because therapists rely heavily on observing facial expressions and body language to assess emotional states and therapeutic rapport.
Timing and availability requirements
Emergency situations demand immediate interpreter access within seconds, making telephonic or VRI your best options. You can’t schedule on-site interpreters when patients arrive unexpectedly in your emergency department or when urgent care visits require instant language support. These remote modes connect you with interpreters 24/7 across hundreds of languages, ensuring no patient waits for critical communication during time-sensitive medical decisions.
Schedule on-site interpreters for planned appointments at least 48 to 72 hours in advance to ensure availability for your needed language and time slot.
Scheduled appointments allow you to arrange on-site interpretation for complex procedures, long consultations, or situations where personal presence enhances the therapeutic relationship. You’ll want on-site interpreters for prenatal visits, cancer treatment planning, discharge planning sessions, or pediatric appointments where multiple family members participate in care discussions.
Cost and resource considerations
Your facility’s budget influences which interpretation modes you deploy most frequently. Telephonic interpretation costs the least per minute while maintaining professional quality standards, making it practical for brief interactions throughout your daily patient flow. VRI requires technology infrastructure but offers faster connection times and visual communication without the travel costs and scheduling constraints of on-site services. On-site interpretation provides the highest quality experience for complex medical encounters but comes with premium pricing and advance scheduling requirements that may not fit every clinical situation.
Best practices when working with interpreters
Working effectively with interpreters requires specific techniques that differ from your usual patient conversations. You need to adjust your communication style, positioning, and session management to ensure accurate patient interpretation flows smoothly between all parties. These practices apply whether you use video, phone, or on-site interpreters, and they directly impact the quality of clinical information you gather and the trust your patient places in the care you provide.
Position interpreters for optimal communication
You should arrange seating so the interpreter sits slightly behind or beside you, forming a triangle with you and your patient. This positioning allows your patient to maintain eye contact with you rather than looking at the interpreter during the conversation. When you use VRI, place the screen where both you and your patient can see the interpreter’s face without turning away from each other. The physical setup reinforces that the therapeutic relationship exists between you and your patient, with the interpreter facilitating rather than mediating the exchange.
Brief interpreters before sessions begin
Professional interpreters arrive prepared, but you enhance accuracy by providing context before the appointment starts. Share the purpose of the visit, any complex medical terms you plan to discuss, and relevant background about your patient’s condition. This briefing takes only 30 to 60 seconds but helps interpreters anticipate specialized vocabulary and prepares them for sensitive topics like terminal diagnoses or mental health assessments. You’ll notice fewer interruptions for clarification when interpreters understand the clinical context upfront.
Brief your interpreter about medical terminology and sensitive topics before the session begins to ensure smoother, more accurate communication throughout the appointment.
Speak directly to your patient
You must address your patient in first person and maintain direct eye contact with them, not the interpreter. Say "How long have you had this pain?" rather than "Ask her how long she’s had this pain." This approach preserves the doctor-patient relationship and keeps your patient engaged as an active participant rather than a passive observer. Pause after each complete thought to allow the interpreter time to convey your message accurately. Short sentences work better than long, complex statements that burden the interpreter’s memory and increase the chance of information loss.
Manage session flow and pacing
You control the appointment pace by speaking at a moderate, steady rate that gives interpreters time to process and convey your words without rushing. Avoid interrupting while the interpreter works, and watch for their hand signals indicating they need you to pause or repeat something. When discussing complex treatment plans or medication instructions, verify your patient’s understanding by asking them to explain back what they heard rather than simply nodding agreement. This teach-back method catches misunderstandings before your patient leaves the facility.
Compliance and accessibility considerations
Your healthcare facility faces strict legal obligations around patient interpretation that go beyond good customer service. Federal laws mandate meaningful access to language services for patients with limited English proficiency and individuals who are deaf or hard of hearing. Understanding these requirements protects your facility from discrimination complaints, civil rights investigations, and potential loss of federal funding while ensuring every patient receives equitable care regardless of their communication needs.
Title VI requirements for language access
Title VI of the Civil Rights Act prohibits discrimination based on national origin at any facility receiving federal financial assistance, which includes most healthcare providers accepting Medicare or Medicaid. You must take reasonable steps to provide meaningful access to your programs and services for LEP patients. This means offering qualified interpreters at no cost to patients, informing patients about available language services through signage and intake materials, and ensuring timely access to interpretation throughout the care continuum.
Your compliance obligations extend to all points of contact with patients, from appointment scheduling and triage through treatment, discharge planning, and billing discussions. You can’t require patients to bring their own interpreters or rely on minor children or untrained family members to interpret medical information. The Department of Health and Human Services Office for Civil Rights enforces these requirements and investigates complaints when facilities deny or delay language services that patients need for meaningful participation in their healthcare.
ADA obligations for deaf and hard-of-hearing patients
The Americans with Disabilities Act requires you to provide effective communication for patients who are deaf or hard of hearing. This typically means offering qualified sign language interpreters for medical appointments, procedures, and consultations where communication matters for safe care delivery. You can’t assume written notes, lip reading, or gesture communication suffices for complex medical discussions, informed consent, or mental health services.
Facilities must provide auxiliary aids and services, including qualified interpreters, unless doing so would fundamentally alter the nature of services or create an undue burden.
Your facility determines which auxiliary aid to use based on the nature, length, complexity, and context of the communication, as well as the patient’s usual method of communication. Video remote interpreting may work for brief interactions, but you should provide on-site ASL interpreters for surgeries, therapy sessions, or lengthy consultations where personal presence enhances communication quality.
Documentation and quality assurance
You need systems for documenting when and how you provided patient interpretation services for compliance audits and quality improvement. Record the language requested, mode of interpretation used, and duration of services in your patient’s medical record. This documentation proves you met your legal obligations and helps you identify patterns in language service utilization across your patient population. Regular quality reviews of your interpretation services ensure interpreters meet professional standards and your patients receive consistent access to qualified language support.
Next steps
Your facility’s approach to patient interpretation affects every LEP and deaf patient who walks through your doors. You’ve learned about the different modes of interpretation, compliance requirements, and best practices that ensure accurate communication during medical encounters. Now you need to evaluate your current language services and identify gaps in coverage, technology infrastructure, or staff training that prevent patients from accessing qualified interpreters when they need them.
Start by reviewing your interpretation service agreements and usage data to see which languages your patient population requires most frequently. Assess whether your current mix of VRI, telephonic, and on-site interpretation matches your clinical needs across emergency, inpatient, and outpatient settings. Then establish protocols that make requesting interpretation services straightforward for your clinical staff.
Languages Unlimited supports healthcare facilities across all 50 states with qualified medical interpreters covering hundreds of languages and dialects. Contact our team to discuss how we can strengthen your patient interpretation services with VRI, telephonic, or on-site support that meets your facility’s specific requirements.